Seasonal affective disorder (SAD) is a form of depression that occurs in the winter months. The symptoms are the same classical depression, the only difference being that it occurs in a seasonal pattern.
SAD is common in the UK and countries north of the equator. Typically the symptoms develop when the hours of daylight start to shorten in September; the symptoms tend to reach a peak in the winter months, December, January and February. Then the severity of symptoms starts to reduce as spring begins and the hours of daylight start to increase.

The symptoms of SAD are the same as the symptoms that occur in depression which include;
• Persistent low mood
• Sadness
• Irritability
• Problems with sleep; difficulty in falling asleep, broken sleep, or excessive sleep
• Low energy levels
• Changes in appetite; it can be reduced or increased which is more commonly seen with SAD
• Loss of pleasure in activities you previously enjoyed
• Hopelessness
• Social isolation
• Difficultly concentrating
• Reduced libido
The symptoms which are more common with SAD compared to normal depression are;
• Difficulty waking up in the morning
• Craving sweet foods and carbs
• Weight gain
• Tiredness
• Low energy

What causes SAD?
The exact cause is not entirely clear, however the most widely accepted theory suggests that SAD is caused by the reduced levels of sunlight in the autumn and winter months, which has an effect on the brain that results in symptoms of depression.
The reduced levels of sunlight affect the way a part of the brain, called the hypothalamus works. The hypothalamus has many important functions; one of those functions involves linking to the nervous system to the endocrine system which is responsible for hormone production.
In the case of SAD, the brain produces increased levels of melatonin, which is the hormone that controls our sleep and wake cycles. It is the increased levels of melatonin results in tiredness and fatigue which are the key symptoms of SAD.

At the same time, reduced levels of sunlight cause a reduction in the production of serotonin in the brain. Serotonin is a hormone that affects our mood, appetite and sleep. It is the low levels of serotonin in the brain result in the “biological” symptoms of classical depression, such as poor sleep, appetite changes, low mood, sadness and lethargy.
The hypothalamus also controls our body’s internal clock known as the circadian rhythm. The body needs sunlight to help regulate the timings of the metabolic functions taking place in the body over a 24 hour period. In some cases, the reduced levels of sunlight in the winter months can disrupt the body’s natural rhythm and as a result the symptoms of SAD can develop.
Getting help
If you have any of the symptoms of SAD and depression it is essential to see your GP for a full assessment.
The good news is the symptoms are treatable and often recognising the symptoms and seeking help is the hardest but most important step to getting the medical attention and support your need to tackle the problem.

Treatment
The National Institute for Health and Care Excellence (NICE) recommend that SAD should be treated in the same way as other forms of depression.
A dual approach of psychological treatments, such as cognitive behavioural therapy (CBT) and anti-depressant medication is often very effective.
Psychological therapies
Talking therapies, such as cognitive behavioural therapy (CBT) involves reflecting on how certain thoughts results in behaviours and help you to develop strategies to help manage your thoughts and feeling in certain situations.
Medication
The preferred type of anti-depressant medication is a group of medication known as SSRI’s (selective serotonin reuptake inhibitors). These medications would be increasing the level of serotonin in the brain which helps to elevate mood and reduce the symptoms of depression.
Lifestyle changes
Although often forgotten, small changes in lifestyle can give significant results, especially in the treatment and prevention of SAD in the long term.
The simple steps you can take to help improve your symptoms are;
Try to get as much sunlight during the day as possible. Walking to and from work, and making sure you leave the office at lunchtime rather than eating at your desk can help increase your hours of sunlight.
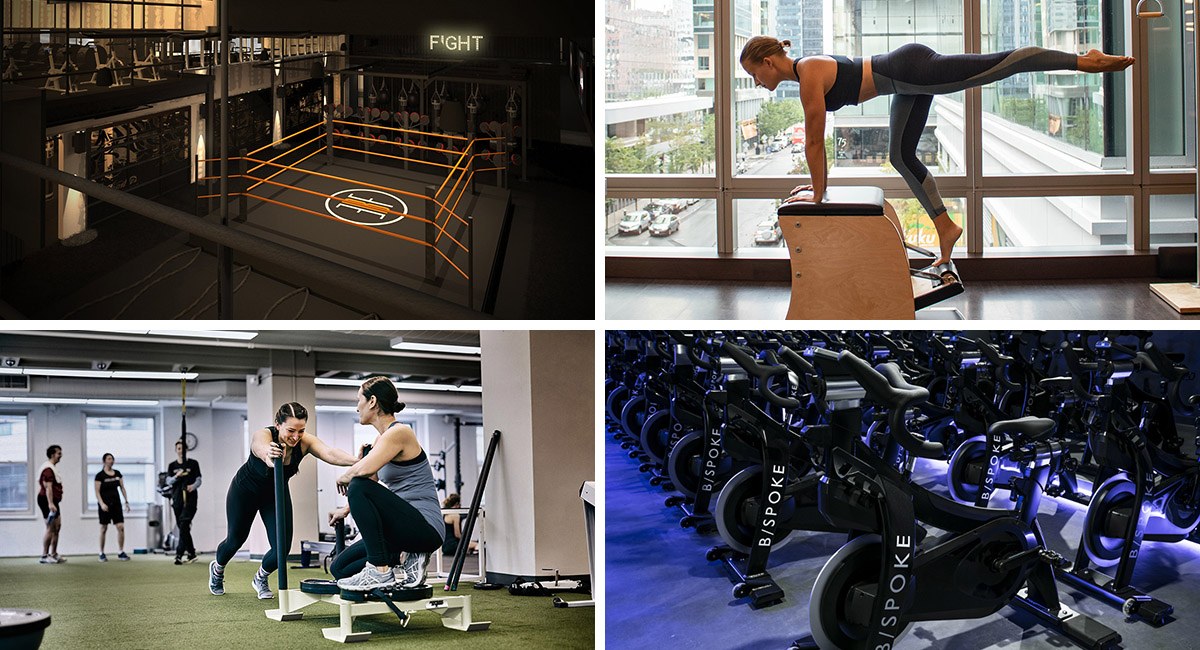
Exercise releases natural endorphins. This gives a natural elevation in mood, hence why exercise is a well-recognised beneficial lifestyle choice in patients with depression. Opting to exercise outside also will optimise your sunlight exposure.
Try to sit near windows and in well-lit rooms especially when working during the day.
Other general lifestyle improvements include;
• Eat a healthy and balanced diet
• Stress relief
• Relaxation techniques
• Mindfulness
Light therapy
Although it may sound like too simple of a solution, people suffering from SAD report that using a special type of light source, called a light box, can significantly improve their mood.
The theory is that artficial light produced by the light box replaces the reduced levels of sunlight we are exposed to during the dark winter months. The light boxes are made in many different designs that can easily integrate into your home environment. Dawn stimulating alarm clocks, which gradually light up your bedroom as you wake up, may also be useful, especially in people who find waking up in the dark a struggle.

The main purpose of the light box is to emit very bright light. However bright the light is, the light is safe because it has special filters built-in to remove harmful UV radiation, so there is no potential risk to the skin or eyes.
Unfortunately, light therapy is not available on the NHS. However is it important you consult with your doctor before investing in a light box to ensure that there are no underlying medical conditions which would mean exposure to a bright light source would be unsuitable for you.

Summary
• SAD is a form of depression, which is seasonal; occurring in autumn and winter and resolving in spring and summer.
• It shares the same symptoms of classical depression, but tiredness, difficulty waking, craving sweet and starchy foods and weight gain are common features predominately seen in SAD.
• The underlying cause is unknown, but it thought to be due to the effects of decrease levels of sunlight on the brain which increase the levels of melatonin and decrease the levels of serotonin.
• SAD is treated in the same way as other forms of depression; with anti-depressant medication and talking therapies.
• Light box therapy is also beneficial, especially when combined with other lifestyle adaptations.
• Visit your doctor for a thorough assessment and to initiate the most appropriate treatment for you.
Dr Jane Leonard
MBCHB. BSC HONS (1ST ) MRCGP
104 Harley Street, London W1G 7JD

Dr Jane Leonard is a fully qualified GP and Cosmetic doctor, graduating from the University of Manchester. She also has a first class honours degree in anatomical sciences, in which she focused her studies on the anatomy of the face, head and neck.
She completed her aesthetic training on Harley Street following a stint at The Alfred Hospital Medical Research Centre, in Melbourne, Australia. Her work in Dermatology research has been published in the prestigious Australasian Journal of Dermatology.
Almost a decade of aesthetic treatment experience, Dr Leonard has been nominated for the Cosmetic Doctor of the Year in the prestigious Safety in Beauty Diamond Awards.